Parkinson’s disease is a progressive neurodegenerative disorder, affecting more than 10 million people worldwide. There are several theories on the cause of Parkinson’s Disease and there are a variety of treatments available today. Deep brain stimulation for Parkinson’s Disease is a surgical approach to manage Parkinson’s symptoms and improve the quality of life of Parkinson’s patients.
Deep brain stimulation, also known as DBS, began in the late 1980s when Alim Benabid identified that electric stimulation of the basal ganglia improved Parkinson’s disease symptoms. Since the late 1980s, many advancements to deep brain stimulation have been made. In 1997, DBS was approved by the FDA as a treatment for Parkinson’s Disease.
Deep brain stimulation is typically reserved for Parkinson’s patients that are in the more advanced stages of the disease process. Early in the progression of Parkinson’s disease, most Parkinson’s patients respond well to L-Dopa containing medications. After years of medication use, the same Parkinson’s medications may no longer provide the same amount of relief. In this case, deep brain stimulation may offer a benefit to help relieve Parkinson’s symptoms and improve the quality of life.
WHAT EXACTLY IS DEEP BRAIN STIMULATION?
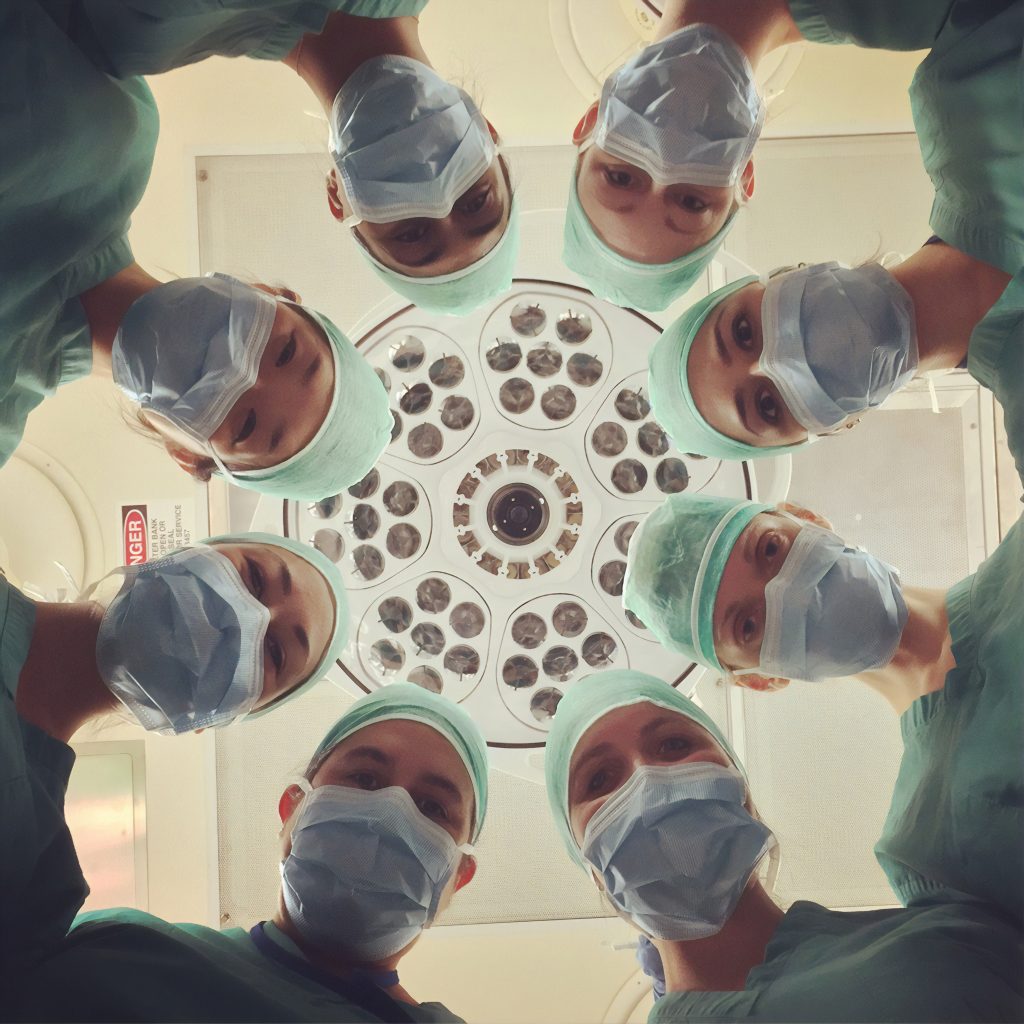
Deep Brain Stimulation is the surgical implantation of electrodes to specific parts of the brain. The implanted device is then connected to a pacemaker-like machine that is implanted underneath the skin of the upper chest. This “pacemaker” allows electrical charges to be delivered to the electrodes in the brain, which results in more firing of the neurons in the areas of the brain that have been damaged.
The two common areas of the brain that are targeted are called the subthalamic nucleus (STN) and the globus pallidus (GPi). Deep brain stimulation to the subthalamic nucleus and globus pallidus can both improve motor functions and improve quality of life. DBS to the subthalamic nucleus typically allows for more reduction in the dose of Parkinson’s medications. DBS to the globus pallidus may result in fewer neurocognitive declines after surgery. Both STN and GPi DBS offer similar benefits to motor symptoms, but also have some subtle differences in results. The selection of DBS location should be carefully considered with a team of healthcare professionals and should be tailored to each patient’s specific case.
IS DEEP BRAIN STIMULATION RIGHT FOR ME?
Deep brain stimulation may be a good option for you, but it is not the best option for everyone. Before any individual is considered for the DBS surgery, he/she must go through a comprehensive assessment with a specialist or team of specialists that can thoroughly evaluate a patient’s medical case.
DBS may not be considered if a patient’s symptoms are well controlled with his/her medication regimen.
DBS may be a good consideration for patients who satisfy one or more of the following:
- Daily doses of L-Dopa exceed a total of 1200mg per day.
- Parkinson’s Disease symptoms are not managed well despite taking appropriate Parkinson’s medications.
- Parkinson’s symptoms are markedly diminishing quality of life.
- Presence of abnormal movements known as dyskinesias that are not improving.
Deep Brain Stimulation can be very useful as a tool for improving the quality of life for many Parkinson’s Disease patients. A team of health care providers can help you determine if it is the right course of action for you.

BENEFITS OF DEEP BRAIN STIMULATION FOR PARKINSON’S DISEASE
Let us discuss the specific benefits that can be achieved with Deep Brain Stimulation for Parkinson’s Disease. Although DBS surgery does not halt the progression of Parkinson’s Disease, DBS surgery can be a powerful benefit for the right candidate.
The benefits of DBS surgery can include the following:
- Motor function improvement for 10 years or possibly longer.
- This can include improvement in tremor, walking, balance, slowness and/or stiffness.
- Long term improvement of daily activities like dressing and/or running errands.
- High patient satisfaction rate. (In one study of 400 patients that have received DBS surgery, over 90% of patients reported they were happy with their decision for deep brain stimulation.)
- DBS electrical stimulation is adjustable and also reversible if a patient experiences any negative consequences of stimulation.
RISKS OF DEEP BRAIN STIMULATION FOR PARKINSON’S DISEASE
DBS surgery is not without risks. Risks include those common to all brain surgeries such as:
- Complications from surgery include infection (most common) and brain hemorrhage.
- Hardware-related complications like the movement of leads, battery failure, and complications with the device. This can require further surgeries to repair.
- Adjustment period after receiving the DBS surgery.
- During the first year of recovery from the surgery, the overseeing medical team will make adjustments in medications and device settings. This can be a delicate process that may require several adjustments. A patient can experience a variety of symptoms during this time due to over- or under-stimulation of the electrodes.
As with any surgery, there are risks to deep brain stimulation surgery. However, these risks are reduced by the surgical experience of the surgeon.
CONCLUSION
Deep brain stimulation can offer some much-needed relief for Parkinson’s disease patients. Although DBS surgery has promising results for many Parkinson’s patients, it may or may not be the best option for treatment. The benefits and risks should be evaluated with a team of specialists to help determine if DBS surgery is a good option for any individual.
Author:
Dr. Darlyn Dragg, N.D.
This article is not intended to diagnose or treat any individual with Parkinson’s Disease or any individual who experiences hallucinations. This article was created for educational purposes only and is not a substitute for medical, psychological or any other sort of professional care. Please always contact your medical provider with any questions or concerns involved treatment for hallucinations and Parkinson’s Disease.
If you have any questions about Parkinson’s Disease or Parkinson’s Disease Treatments, please contact The Parkinsons Plan at 603-677-1484